|
Case Series
Heterodigital neurovascular island flap is a sensible solution for severe soft tissue defect of the thumb: A case series
1 Staff of Department of Orthopaedic and Traumatology, Faculty of Medicine and Nursing, Yogyakarta, Indonesia
2 Resident of Department of Orthopaedic and Traumatology, Faculty of Medicine and Nursing, Yogyakarta, Indonesia
Address correspondence to:
Reza Muttaqien
Resident of Department of Orthopaedic and Traumatology, Faculty of Medicine and Nursing, Yogyakarta 55211,
Indonesia
Message to Corresponding Author
Article ID: 100015O03M2019
Access full text article on other devices
Access PDF of article on other devices

How to cite this article
Meirizal, Muttaqien R. Heterodigital neurovascular island flap is a sensible solution for severe soft tissue defect of the thumb: A case series. Edorium J Orthop 2019;5:100015O03M2019.ABSTRACT
Introduction: The thumb plays a major role in hand function. Injury to the thumb greatly affects the function of the hands compared to the injury occurring to other fingers. Efforts to bring back thumb’s mobility, length, stability, and sensory properties after hand trauma are of extreme priority. Devascularized digits with segmental skin and vessel loss require revascularization and resurfacing. This can be done by using the heterodigital vascular island flap which gives appropriately sized pristine artery of optimal length for revascularization and provides simultaneous skin cover. Reconstructive objectives are preserving the length, restoring function, sensation, and presentation. The disadvantage from the flap is the probability of cold intolerance in the digit from loss of pedicle artery.
Case Report: We report two cases in which heterodigital neurovascular island flap was used. Primary wound healing was achieved in all patients with good functional recovery of the thumb, acceptable donor site morbidity, and improvement in hand functional scoring based on Quick DASH.
Conclusion: The heterodigital neurovascular island flap is excellent both aesthetically and functionally for reconstruction of the thumb defect.
Keywords: Heterodigital neurovascular island flap, Thumb defect, Thumb reconstruction, Quick DASH
INTRODUCTION
Traumatic injuries to the thumb are extremely common in the hand [1]. Injuries can result in soft tissue loss associated with vessel injuries necessitating revascularization, in addition to soft tissue coverage [2]. The thumb tip is the end organ for touch, which is packed with special sensory receptors that enable hand to perceive touch. Complex damage to the thumb tip results in loss of fingertip sensibility which gives challenging problems for hand surgeons [1]. Reconstructive objectives are preserving length, restoring function, sensation, and presentation. The thumb plays vital roles in hand function to do daily activities such as gripping, holding, opposition, circumduction, and motions. Therefore, injury to the thumb greatly affects the function of the hands compared to the injury occurring to other fingers [3].
An interpositional vein graft for revascularization followed by soft tissue coverage using local, regional, or a free flap is traditionally used. Literature has described the use of a free flow through flap that permits simultaneous revascularization and coverage [2]. Among numerous reconstructive options, one has to choose an option which results in pain-free fingertip with durable, sense-perceiving skin cover. Heterodigital vascularized island flap has more advantages, such as functionally restore large soft tissue defects in a single stage, can be optimally used for digits of unequal length so that the donor thumb tip is not violated, also does not require immobilizing digits with possible donor and recipient finger stiffness and contractures and enables early postoperative mobilization. In contrast with cross finger flap which involves immobilizing digits in an unnatural position, with results in possible donor and recipient finger stiffness and contracture [1].
CASE REPORT
Case 1
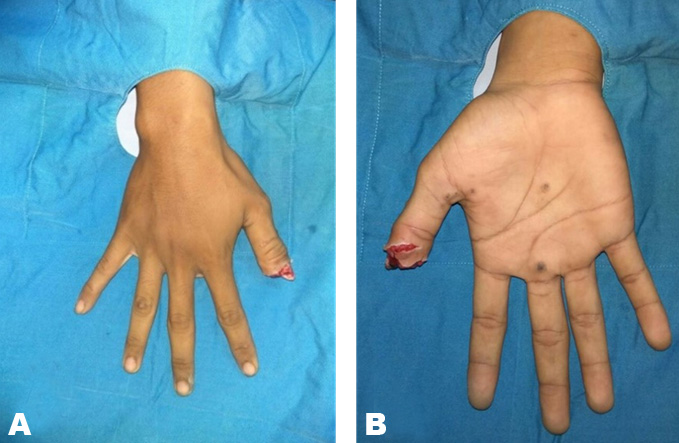
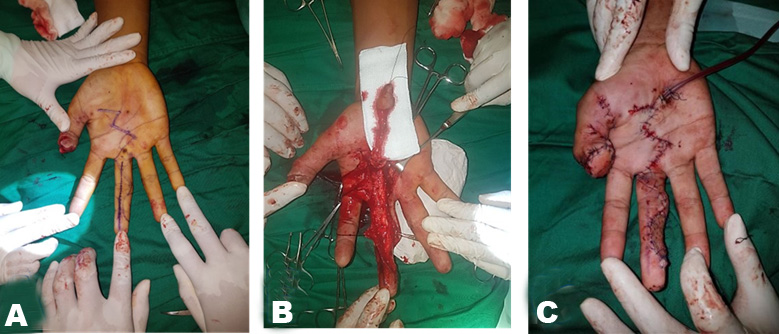
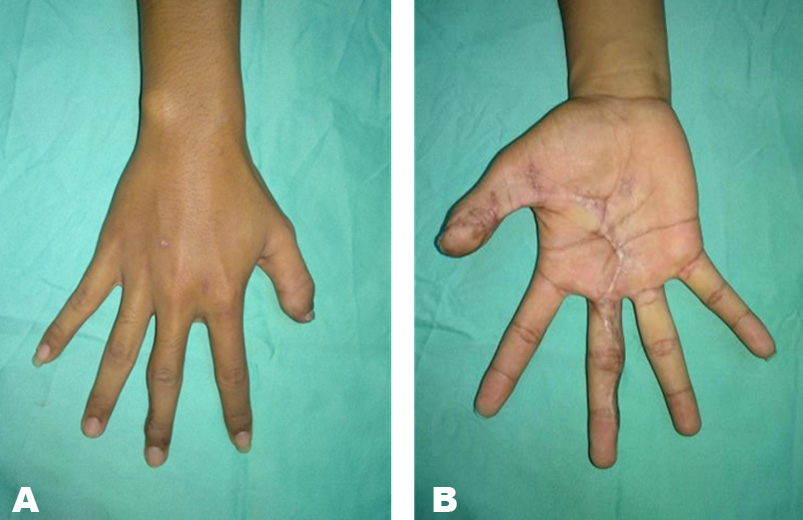
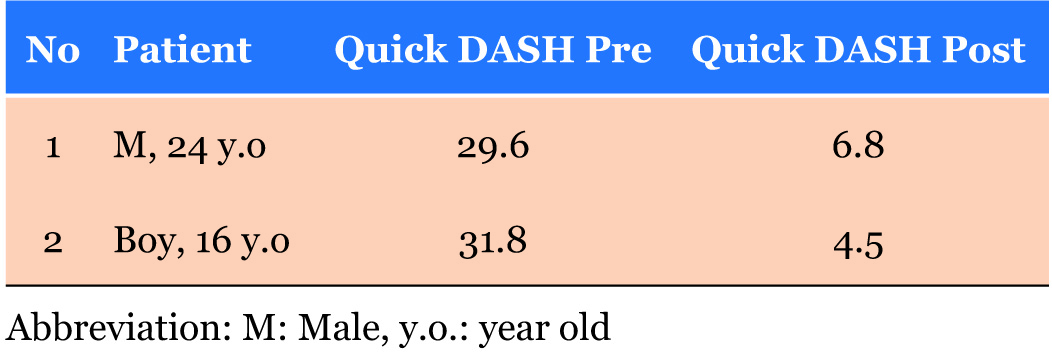
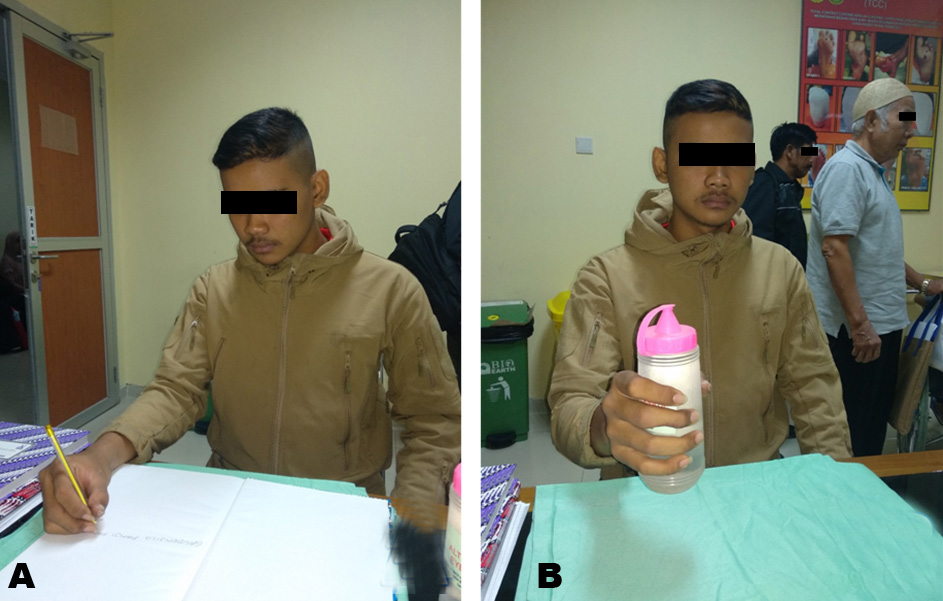
A 24-year-old right-handed man, college student suffered from an avulsion amputation of his right thumb when it got caught in a motorcycle gear. Upon examination, it was found that there was soft tissue loss at the level of distal interphalanx of the thumb, loss of pulp, nail bed, thrombosis of both digital arteries, and fracture of distal phalanx (Figure 1). A heterodigital vascular island flap, raised from the ulnar aspect of the middle finger was used to revascularize the thumb and resurface the 2.5–1.5 cm defect over the distal finger (Figure 2). The donor defect on the middle finger was resurfaced with a full thickness skin graft from the inguinal region. After two months follow-up good soft tissue cover with an adequate skin of color and texture similar to contralateral thumb was achieved. Flap showed excellent viability with no flap loss, partial necrosis, or superficial sloughing. Sensibility was preserved with a static two point discrimination (TPD) ranging from 2 to 4 mm. It was shown to be almost comparable to the TPD of the contralateral normal finger. No progressive deterioration insensibility was noticed after more than three months follow-up (Figure 3). There was no donor site morbidity, hypoesthesia, hyperpigmentation, and cold intolerance of the ulnar aspect of the donor digit. On follow-up four months later, the flap was well settled and the patient returned to perform the daily living activity with postoperative Quick DASH score 3 (Table 1) (No level of difficulty with excellent functional outcome) (Figure 4).
Case 2
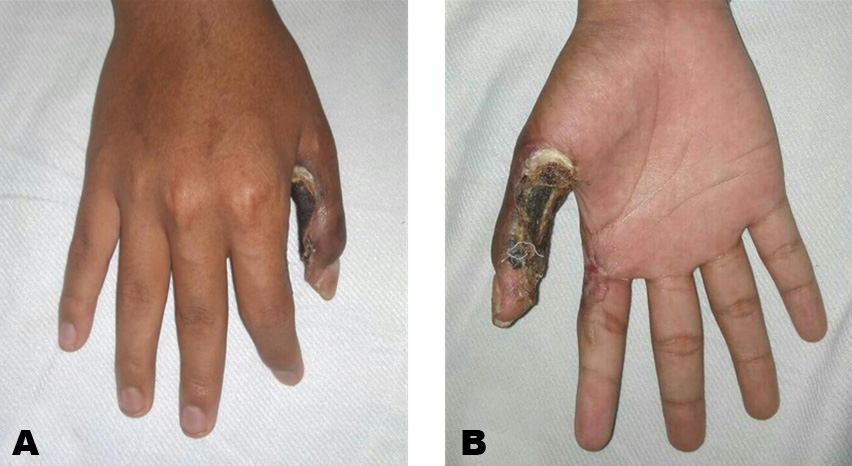
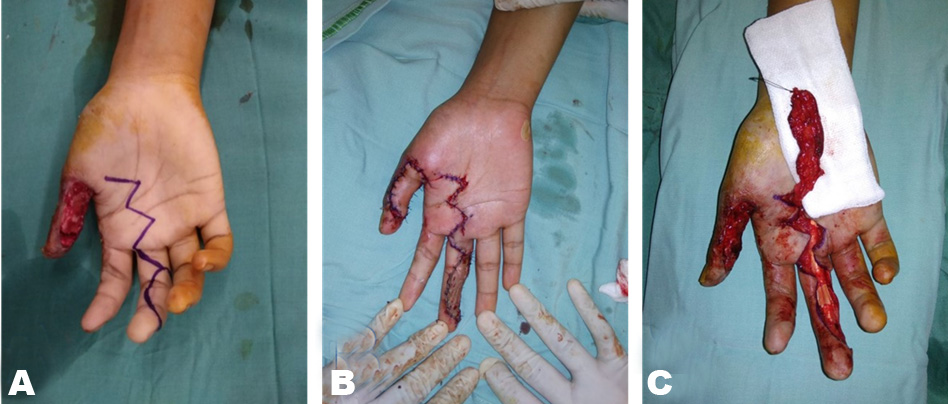
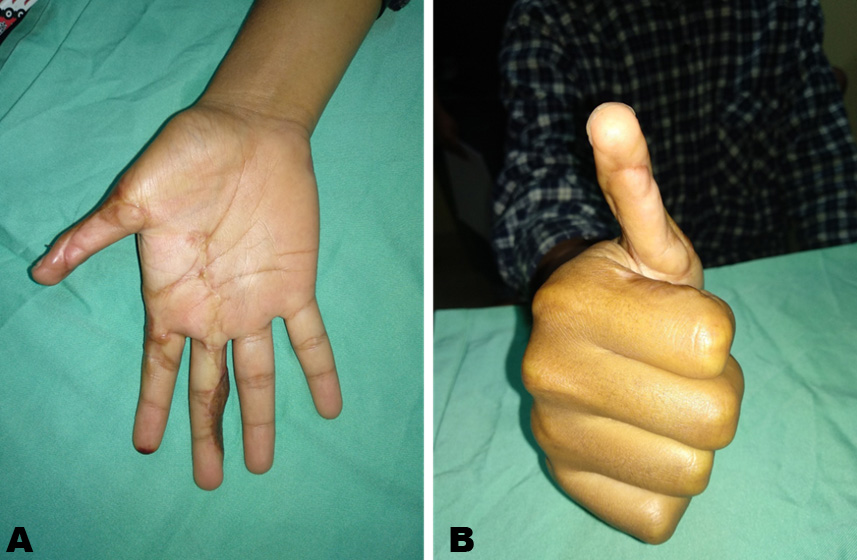
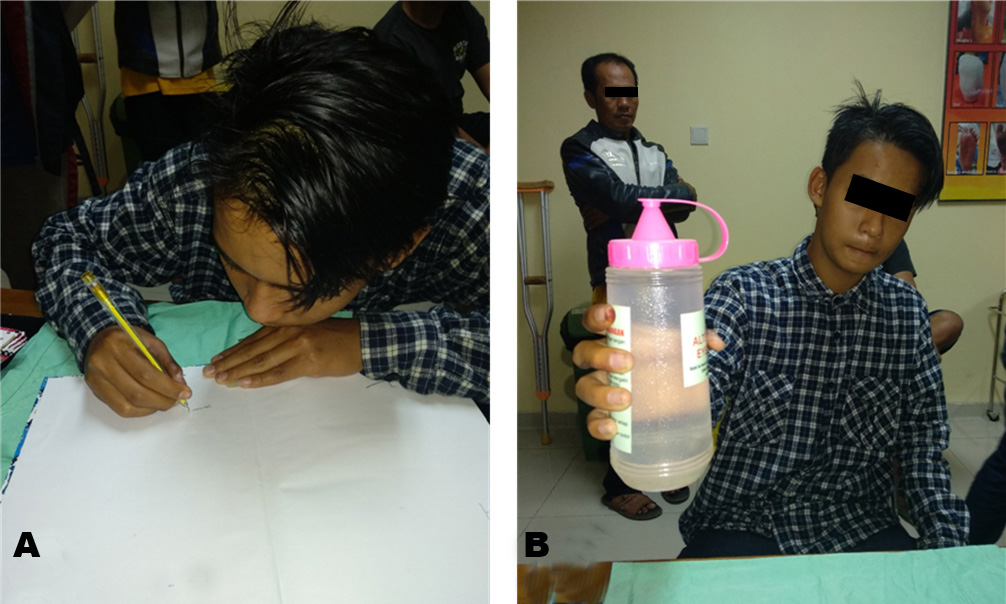
A 16-year-old left-handed boy, senior high school student suffered from an electric burn injury to his left thumb when it came in contact with an electrical cord. Upon examination, he had a soft tissue loss with a necrotic wound over the volar aspect of the thumb, joint stiffness, and extension contracture of proximal interphalangeal (PIP) and distal interphalangeal (DIP) joint, with preoperative Quick DASH score 25 (Moderate level of difficulty with fair functional outcome) (Figure 5). After debridement, a heterodigital vascular island flap raised from the ulnar aspect of the middle finger was used to revascularize the thumb and resurfaced the 3.5–2.5 cm defect over the finger. The donor defect on the middle finger was resurfaced with a full thickness skin graft from the inguinal region (Figure 6). After two months follow-up good soft tissue cover with an adequate skin of color and texture similar to contralateral thumb was achieved. Flap showed excellent viability with no flap loss, partial necrosis, or superficial sloughing with fusion of interphalanx joint. Sensibility was preserved with a static TPD ranging from 3 to 6 mm. It was shown to be almost comparable to the TPD of the contralateral normal finger. No progressive deterioration in sensibility was noticed after more than three months of follow-up. There was no donor site morbidity, no hypoesthesia, hyperpigmentation, and cold intolerance of the ulnar aspect of the donor digit (Figure 7). On followup five months later, the flap was well settled and the patient returned to perform the daily living activity with postoperative Quick DASH score 3 (No level of difficulty with excellent functional outcome) (Table 1). However, he had a contracture of the PIP and DIP joint due to the history of soft tissue damage and fusion of interphalanx joint (Figure 8).
DISCUSSION
Damage to the fingertip (injury distal to the insertion of the flexor and extensor tendons) is common, above all, in young men who perform manual labor [4]. Diagnosis is achieved immediately, based on clinical history and examination, also from the plain photograph of the damaged digit. The thumb plays a major role in hand function. Efforts to bring back thumb’s mobility, length, stability, and sensory properties after hand trauma are certainly needed to be done [3]. The treatment method is selected with consideration of soft-tissue loss, nail bed integrity, and age and physical demands of the patient. The thumb reconstruction objective is to bring back sensate function to the tip using tissue that mimics volar pulp volume, texture, and contour [1]. The heterodigital neurovascular island flap method is used to achieve this purpose. To enhance sensibility recovery, the flap has been modified by suturing the dorsal digital nerves to the proper digital nerve of the injured finger. This technique was even further improved including both dorsal digital nerves with the aim of achieving better sensory fiber input [5].
Morbidity of the donor site related to the heterodigital island flaps can be reduced by cautiously giving attention to detail. The digital nerve is preserved in continuity, the flap is harvested from the “blind” side of the digit (ulnar side of index/middle finger) and the distal pulp is not harvested. By doing this, the donor finger will maintain a normal sensate pulp. While raising the flap it is vital not to violate the flexion crease of the donor digit. A full thickness skin graft with a tie over dressing allows early mobilization and prevents late contractures and stiffness of joints [1],[2].
Indications for heterodigital island flaps are: (1) Extensive loss of the palmar thumb pulp (more than 1.5 cm), (2) Single stage reconstruction with minimal risk of infection to internal prosthetic devices, (3) Loss of thermal digital nerve innervation, particularly of the ulnar side of thumb, (4) Good choice for older patients (minimal risk of stiffness and contracture). Contraindications in this procedure are crushing or penetrating injury (pedicle vessels may be injured) and severe infections (donor vessels may be compromised) [5],[6].
There are three steps of the heterodigital island flap method which consist of: (1) Preoperative and intraoperative planning including selecting a healthy donor digit, size determination, ensure the pedicle length is long enough and marking a midlateral incision with zigzag pattern, (2) Flap dissection with elevating digital neurovascular structures and release of Cleland ligaments, and (3) Flap insetting and full thickness skin graft (FTSG) donor site [1],[5].
Peraut et al. reported the results of heterodigital island flap in two patients who had traumatic ring avulsion and who had satisfactory two point discrimination and cortical re-orientation. The main complications of this method has been identified as cold intolerance, low somatosensory cortical integration, and diminished discrimination sensibility over time. The donor site morbidity is nearly constant: half-pulp hypoesthesia, trophic disorders, pain, and temperature sensation deficits [1].
CONCLUSION
The heterodigital neurovascular island flap allows coverage of difficult extensive digital defects (>1.5 cm) including the pulp with glabrous, sensitive, supple, and well-vascularized skin in one operative stage. Postoperative rehabilitative treatment should be aimed not only toward achieving the best possible sensory recovery, but also toward reducing problems associated with donor digit healing to the lowest. One limitation of the flap is that it requires to sacrifice an arterial pedicle that may cause cold intolerance in the digit. To conclude, the heterodigital neurovascular island flap is an excellent option for reconstruction of the thumb defect which gives great result both aesthetically and functionally.
REFERENCES
1.
Peraut E, Mirous MP, Chammas M. Secondary restoration of fingertip sensation with Littler’s heterodigital neurovascular island flap after ring avulsion injury: Report of two cases. Chir Main 2015;34(1):49–54. [CrossRef]
[Pubmed]

2.
Pham DT, Netscher DT. Vascularized heterodigital island flap for fingertip and dorsal finger reconstruction. J Hand Surg Am 2015;40(12):2458–64. [CrossRef]
[Pubmed]

3.
4.
Fassler PR. Fingertip injuries: Evaluation and treatment. J Am Acad Orthop Surg 1996;4(1):84–92.
[Pubmed]

5.
Lee DH, Mignemi ME, Crosby SN. Fingertip injuries: An update on management. J Am Acad Orthop Surg 2013;21(12):756–66. [CrossRef]
[Pubmed]

6.
Sahin C, Karagoz H, Sever C, Kulahci Y, Ulkur E. Reconstruction of the great toe tip defect with a pedicled heterodigital artery flap. Aesthetic Plast Surg 2013;37(2):421–3. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Meirizal - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Reza Muttaqien - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2019 Meirizal et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.