|
Case Series
The use of intact fish-skin wrap in preventing adhesions during tendon repair: A report of two cases
1 Chief, Division of Plastic, Reconstructive and Hand Surgery, Richmond University Medical Center, Staten Island, New York, USA
Address correspondence to:
Michael J Lacqua
MD, 2372 Victory Boulevard, Staten Island, NY 10314,
USA
Message to Corresponding Author
Article ID: 100018O03ML2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Lacqua MJ. The use of intact fish-skin wrap in preventing adhesions during tendon repair: A report of two cases. Edorium J Orthop 2021;7:100018O03ML2021.ABSTRACT
Introduction: Adhesion to adjacent soft tissue is the most common complication following repair of a tendon laceration. Despite extensive research in adhesion prevention, no current method has distinguished itself as optimal. A full thickness intact fish skin has a high Omega-3 fatty acid content, shown to have anti-inflammatory properties.
Case Series: Two patients with hand tendon injuries underwent standard repair and tendon wrapping with intact fish skin. Both patients recovered well with no magnetic resonance imaging (MRI) findings of adhesions.
Conclusion: We postulate the fatty acid imparts a protective anti-inflammatory effect against adhesion formation as the wrap is absorbed. Further prospective studies are needed to evaluate the reproducibility of adhesion prevention seen in these isolated cases.
Keywords: Fish-skin wrap, Tendon adhesions, Tendon repair, Tendon repair outcomes
INTRODUCTION
Adhesion to adjacent soft tissue is the most common complication following repair of a tendon laceration within the digital sheath. This leads to hand dysfunction and the need for additional surgery. Many biological and synthetic materials have been employed to prevent such adhesions with varied success. Despite extensive research and application, no current method has distinguished itself as optimal and thus there remains a critical need for further investigation.
Omega-3 fatty acids (FAs) have been shown to have an anti-inflammatory effect. A full-thickness intact fish skin (Kerecis Omega-3 Wound by Kerecis) undergoes very gentle processing during its processing in preparation for its Food and Drug Administration (FDA) approved use in the treatment of chronic wounds. It is shown to have extremely high Omega-3 FA content. Down-regulation of the local inflammatory response surrounding a repaired tendon may reduce or even eliminate the formation of adhesions. Intact fish skin would therefore seem to be an ideal biological wrap to use during tendon repair to protect the site from the development of local adhesions.
CASE SERIES
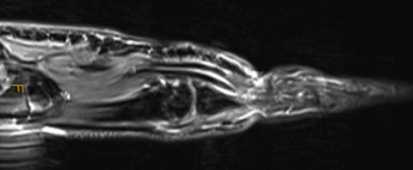
Case #1 is that of a 23-year-old young man with a Zone 2 40% flexor digitorum profundus (FDP) tendon and 70% flexor digitorum superficialis (FDS) tendon laceration to his non-dominant left ring finger (Figure 1). He underwent repair of both tendons with 4.0 prolene core sutures and a wrap of the FDS tendon with the intact fish skin secured to itself with 5.0 chromic suture (Figure 2). No tendon sheath was involved anatomically at the site of the repair. The patient received 1 gram of Ancef intravenously pre-operatively and was maintained post-operatively on Cephalexin orally for five days. Post-operatively, the patient underwent immediate Occupational Therapy consisting of the Modified Duran Program for five weeks.
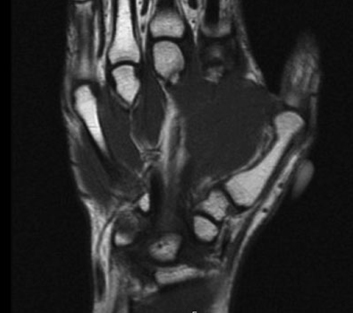
Case #2 is that of a 32-year-old man with a complete laceration in Zone 4 of his left thumb extensor pollicis longus (EPL) tendon (Figure 3). He underwent repair of the tendon with a 3.0 prolene core suture and fish-skin wrap secured to itself with 5.0 chromic suture as well (Figure 4). No tendon sheath was involved anatomically at the site of the repair. The patient received 1 gram of Ancef intravenously pre-operatively and was maintained post-operatively on Cephalexin orally for 5 days. The patient was placed in a fiberglass thumb spica splint post-operatively because he needed to return to work for financial reasons and was not able to partake in any type of therapy. He remained splinted for five weeks and then began a two week course of Occupational Therapy.
At week 6 following surgery Case #1 achieved complete, active, independent range of motion of the ring finger distal and proximal interphalangeal joints (Figure 5). Using the American Society for Surgery of the Hand (ASSH) total active motion (TAM) system, his function was measured at 100% (excellent). At week 6, Case #2 began occupational therapy and after two weeks of therapy he had complete, normal motion of the thumb interphalangeal joint with his results measured at 78% (good).
An MRI performed on both patients on week 6 post-operatively (Figure 6 and Figure 7, respectively) demonstrated absorption of the fish-skin wrap, minimal fluid around the repair sites, and the absence of any peritendinous adhesions.
DISCUSSION
Prevention of tendon adhesions following tendon laceration repair continues to be a challenging issue to hand surgeons. Great advances have been made in surgical technique and occupational therapy protocols to improve tendon gliding post-operatively to reduce the incidence of adhesions and the need for secondary surgery. Additionally, many biologic and synthetic materials have been employed as tendon wraps in the hopes of reducing the formation of adhesions. A multi-layer electrospun membrane (PELA) showed potential in promoting tendon gliding without impairing tendon healing [1]. An ibuprofen-loaded hyaluronic acid nanofibrous membrane wrap showed promise in preventing peritendinous adhesions after tendon surgery seemingly due to its anti-inflammatory effects [2]. Biological amnion wraps were shown in a multicenter clinical trial to result in reduced complications in tendon repair surgery including a lower tendon adhesion rate [3]. Chen et al. showed that transcription factor RelA/p65 inhibition prevents tendon adhesions by modulating inflammation, cell proliferation, and apoptosis [4]. Waterborne biodegradable polyurethane films have also shown potential in anti-adhesion applications [5]. All these modalities and techniques have been met with various degrees of success. The ideal material, however, remains elusive.
The intact fish skin used as a wrap for the two patients presented is a product of North Atlantic codfish. It has a structure and chemical composition very similar to that of human skin [6]. Unlike many other mammalian-derived dermal matrix products that require harsh detergent and chemical processing prior to application in humans, the intact fish skin only needs to be gently processed prior to use because of the absence of a viral transmission risk [7]. This allows the fish-skin structure and bioactive composition, notably lipids, to be preserved. The intact fish skin is found to be rich in Omega-3 FAs, especially eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) [8]. It is these FAs that have been shown to down-regulate inflammation [9]. This occurs due to inhibition of leucocyte chemotaxis, adhesion molecule expression, leucocyte-endothelial adhesive interactions, the production of prostaglandins and leukotrienes, and the production of pro-inflammatory cytokines [10]. Mechanisms underlying the anti-inflammatory actions of EPA and DHA include altered cell membrane phospholipid fatty acid composition, the disruption of lipid rafts, inhibition of activation of the pro-inflammatory transcription factor nuclear factor beta, and activation of the anti-inflammatory transcription factor peroxisome proliferation-activated receptor gamma [10].
We postulate that the FAs present within the intact fish skin and preserved during the gentle processing are reconstituted and slowly released at the tendon repair site as the wrap is absorbed. This imparts the established anti-inflammatory effects of FA leading to the apparent absence of adhesion formation in these two patients. It seems to be effective in both partial and full thickness tendon injuries.
CONCLUSION
These are the first reported cases of using intact fish skin during the repair of both partial and complete traumatic tendon lacerations in the hope of preventing adhesions. We have used a similar technique in five additional cases of both partial and complete tendon laceration with similar results. Further prospective studies are needed and are being designed, however, to evaluate the reproducibility of adhesion prevention seen in these isolated cases.
REFERENCES
1.
Jiang S, Yan H, Fan D, Song J, Fan C. Multi-layer electrospun membrane mimicking tendon sheath for prevention of tendon adhesions. Int J Mol Sci 2015;16(4):6932–44. [CrossRef]
[Pubmed]

2.
Chen CT, Chen CH, Sheu C, Chen JP. Ibuprofen-loaded hyaluronic acid nanofibrous membranes for prevention of postoperative tendon adhesion through reduction of inflammation. Int J Mol Sci 2019;20(20):5038. [CrossRef]
[Pubmed]

3.
Lun C, Bai J, Yu k, Liu G, Tian S, Tian D. Biological amnion prevents flexor tendon adhesion in zone II: A controlled, multicentre clinical trial. Biomed Res Int 2019;2019:2354325. [CrossRef]
[Pubmed]

4.
Chen S, Jiang S, Zheng W, et al. RelA/p65 inhibition prevents tendon adhesion by modulating inflammation, cell proliferation, and apoptosis. Cell Death Dis 2017;8(3):e2710. [CrossRef]
[Pubmed]

5.
Hsu SH, Dai LG, Hung YM, Dai NT. Evaluation and characterization of waterborne biodegradable polyurethane films for the prevention of tendon postoperative adhesion. Int J Nanomedicine 2018;13:5485–97. [CrossRef]
[Pubmed]

6.
Rakers S, Gebert M, Uppalapati S, et al. ‘Fish matter’: The relevance of fish skin biology to investigative dermatology. Exp Dermatol 2010;19(4):313–24. [CrossRef]
[Pubmed]

7.
Crapo PM, Gilbert TW, Badylak SF. An overview of tissue and whole organ decellularization processes. Biomaterials 2011;32(12):3233–43. [CrossRef]
[Pubmed]

8.
Kotronoulas A, Jónasdóttir HS, Sigurðardóttir RS, Halldórsson S, Haraldsson GG, Rolfsson Ó. Wound healing grafts: Omega-3 fatty acid lipid content differentiates the lipid profiles of acellular Atlantic cod skin from traditional dermal substitutes. J Tissue Eng Regen Med 2020;14(3):441–51. [CrossRef]
[Pubmed]

9.
Serhan CN. Pro-resolving lipid mediators are leads for resolution physiology. Nature 2014;510(7503):92–101. [CrossRef]
[Pubmed]

10.
Calder P. Omega-3 fatty acids and inflammation processes: From molecules to man. Biochem Soc Trans 2017;45(5):1105–15. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Michael J Lacqua - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthor declares no conflict of interest.
Copyright© 2021 Michael J Lacqua. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.