|
Research Article
Medium term results after in situ screw fixation of slipped capitis femoral epiphysis: A 33 case series
1 Paediatric and Orthopaedic Surgical Department, Istituto Pediatrico della Svizzera Italiana IPSI, Bellinzona and Valli Regional Hospital, Ticino, Switzerland
Address correspondence to:
Marco Odorizzi
Paediatric and Orthopaedic Surgical Department, Istituto Pediatrico della Svizzera Italiana IPSI, Bellinzona and Valli Regional Hospital, Ticino,
Switzerland
Message to Corresponding Author
Article ID: 100019O03MO2021
Access full text article on other devices
Access PDF of article on other devices

How to cite this article
Odorizzi M, De Rosa V, Mameli A. Medium term results after in situ screw fixation of slipped capitis femoral epiphysis: A 33 case series. Edorium J Orthop 2021;7:100019O03MO2021.ABSTRACT
Aims: Hip epiphysiolysis is a disease that affects children and teenagers during their growth and is normally treated surgically with reduction and percutaneous fixation to prevent further displacement of the epiphysis and the related complications. The aim of this study was to evaluate the outcome of the surgical treatment of hip epiphysiolysis with a single percutaneous screw.
Methods: Thirty-three patients, treated at the authors’ institution, with a mean age at surgery of 12.4 years and a male/female ratio of 60% were included in this retrospective case series. The right hip was involved in 11 patients, the left hip in 19 patients, and a bilateral involvement was present in 3 patients. All patients were treated with a percutaneous fixation of the slipped epiphysis with a single screw. Results: After a mean follow-up of 7.7 years, the mean Oxford hip score was 47.2. All patients regained a full range of motion. Eleven of them were fully satisfied with the treatment whereas 1 patient was partially satisfied. No complications were reported, neither intra-operatively, nor post-operatively, and no re-interventions were needed.
Conclusions: Percutaneous fixation of the slipped epiphysis with a single screw guarantees good functional outcomes and high patients’ satisfaction without relevant complications. Thus, it can be considered a safe and effective procedure for the treatment of hip epiphysiolysis.
Keywords: Hip epiphysiolisis, Percutaneous fixation, SCFE
INTRODUCTION
Epiphysiolysis of the femoral head is the most frequent hip injury in children, aged 9 to 15 [1]. This pathology is defined as the slipping of the proximal femoral epiphysis on the metaphysis through the growth cartilage. In this location the metaphysis translates anteriorly and rotates externally, while the epiphysis remains in the acetabulum and therefore is posterior to the metaphyseal region [1],[2].
From an epidemiological point of view, the disease has a prevalence of 10/100,000 children, it is more frequent in males than in females, the ratio is between 1.1:1 and up to 4.1:1, in specific ethnic groups such as African Americans, Latins, or Pacific Islanders. The average age at diagnosis is 13.5 years for males and 12.0 years for females; it is present bilaterally in 18–50% of patients. Furthermore, it appears that there is a different incidence rate of the disease depending on the seasons, with an increase in cases during the summer months due to a likely increase in physical activity [2].
The etiological agent of the disease is multifactorial. Identified biomechanical factors are obesity, increase in femoral and/or acetabular retroversion and increase in the inclination of the physes; all these conditions they produce an increased transversal cutting force at the level of the femoral head and therefore favor the onset of the pathology. Epiphysiolysis is also known to be associated with endocrine disorders such as hypothyroidism, growth hormone deficiency, hypogonadism, and hypopituitarism. Other patients at greater risk of developing the disease are those with osteodystrophy from renal failure or those who have undergone radiotherapy of the pelvis [2],[3].
Different classifications for epiphysiolysis have been proposed, depending on the ability to bear the weight of the body, the duration of the symptoms, the size of the epiphyseal angle and the percentage of slippage [4].
The most used one is Loder Classification which distinguishes the pathology in stable, when the patient is able to bear the weight of the body with or without crutches and that has less risk of osteonecrosis of the femoral head (<10%), or unstable, when the patient is unable to walk and with a high risk of osteonecrosis (about 30–40%). The second most used classification is the Grading System which distinguishes the epiphysiolysis in three degrees according to the percentage of slipping of the femoral head; First degree includes 0–33% of slippage, Second degree 34–50%, and Third degree >50%. Another parameter that is taken into consideration in hip epiphysiolysis is the measurement of the Southwick angle; in this circumstance the value found can be distinguished between mild (<30°), moderate (30–50°) or severe (>50°) disease. The diagnosis of the disease is initially clinical, subsequently needs support radiology.
The most common symptom of epiphysiolysis is pain. Algic symptoms are generally localized in the affected hip but can also be present in other locations, such as the thigh or knee. Pain in the knee or distal femur is a symptom that occurs in the 15–50% of patients and can lead to a delay in diagnosis. Generally, it is associated with no notion of previous traumatic hip event [2],[3],[4],[5].
Objectively, the patient presents abnormal gait with lower limb in external rotation and decreased excursion movement of the affected hip, up to presenting lameness free. There is a positive Drehmann sign associated with loss of intrarotation, hip abduction, and flexion. Unless the patient is suffering from bilateral epiphysiolysis, it is very useful to compare range of motion (ROM) with the contralateral hip; in more advanced cases there may also be an atrophy of the thigh muscles from non-use.
As far as the radiological aspect is concerned, the reference examination is the X-ray that must be performed in double (AP and frog-leg lateral views) and bilateral projection [1],[2]. On the antero-posterior (AP) profile it is possible to diagnose evident epiphyseal slips or, for less striking cases, it allows to trace the Klein’s line in order to show at what level the proximal femoral epiphysis is crossed. On the frog-leg lateral view profile, it is possible to measure the epiphyseal angle using the Southwick method.
A further radiological examination that can be performed in epiphysiolysis is magnetic resonance imaging (MRI) which could help diagnose patients with minimal dislocations and negative radiography; it also allows to identify cases of pre-slipping, increase in size of growth cartilage or presence of metaphyseal edema.
Early diagnosis is extremely important as the prognosis of the disease is closely related to the speed with which it is diagnosed and treated. Delays in diagnosis can lead to disabling conditions and degenerative osteoarthritis of the hip early onset which would inevitably lead to joint reconstruction.
The treatment of this pathology is a controversial topic and aims to prevent further slippage and avoid complications, such as chondrolysis and avascular necrosis [2],[3],[4],[5],[6].
Percutaneous in situ fixation is currently the most frequently used technique and has shown good results [4],[6],[7],[8]. The use of one or two cannulated screws is controversial; the double screw guarantees a more stable construct but exposes the bone to greater “trauma” with greater risk of joint penetration. In general, the percutaneous fixation technique limits the risk of necrosis and chondrolysis, but leaves a persistent deformity at the level of the head-neck junction that can be responsible for the intermediate and long-term evolution of the femoroacetabular impingement and subsequent arthrosis. As regards this deformity, many authors who support fixation in situ believe that metaphyseal remodeling occurs over time and that residual deformity has no clinically significant long-term consequences [4]. Other authors, however, question this remodeling potential and recommend more complex surgery.
Among these interventions, a technique that guarantees the best result in terms of anatomy and therefore limits the risk of impingement is Dunn’s subcapital osteotomy; the indication for the realization of this technique is a severe slipping of the femoral head, absence of osteoarthritis or osteonecrosis and important pain or functional limitation due to deformity. The limitations of this technique are that it is very invasive and increases the risk of femoral head necrosis [7].
Our monocentric retrospective study aims to have both medium- and long-term clinical and radiological results in the surgical treatment of epiphysiolysis with a single percutaneous screw.
MATERIALS AND METHODS
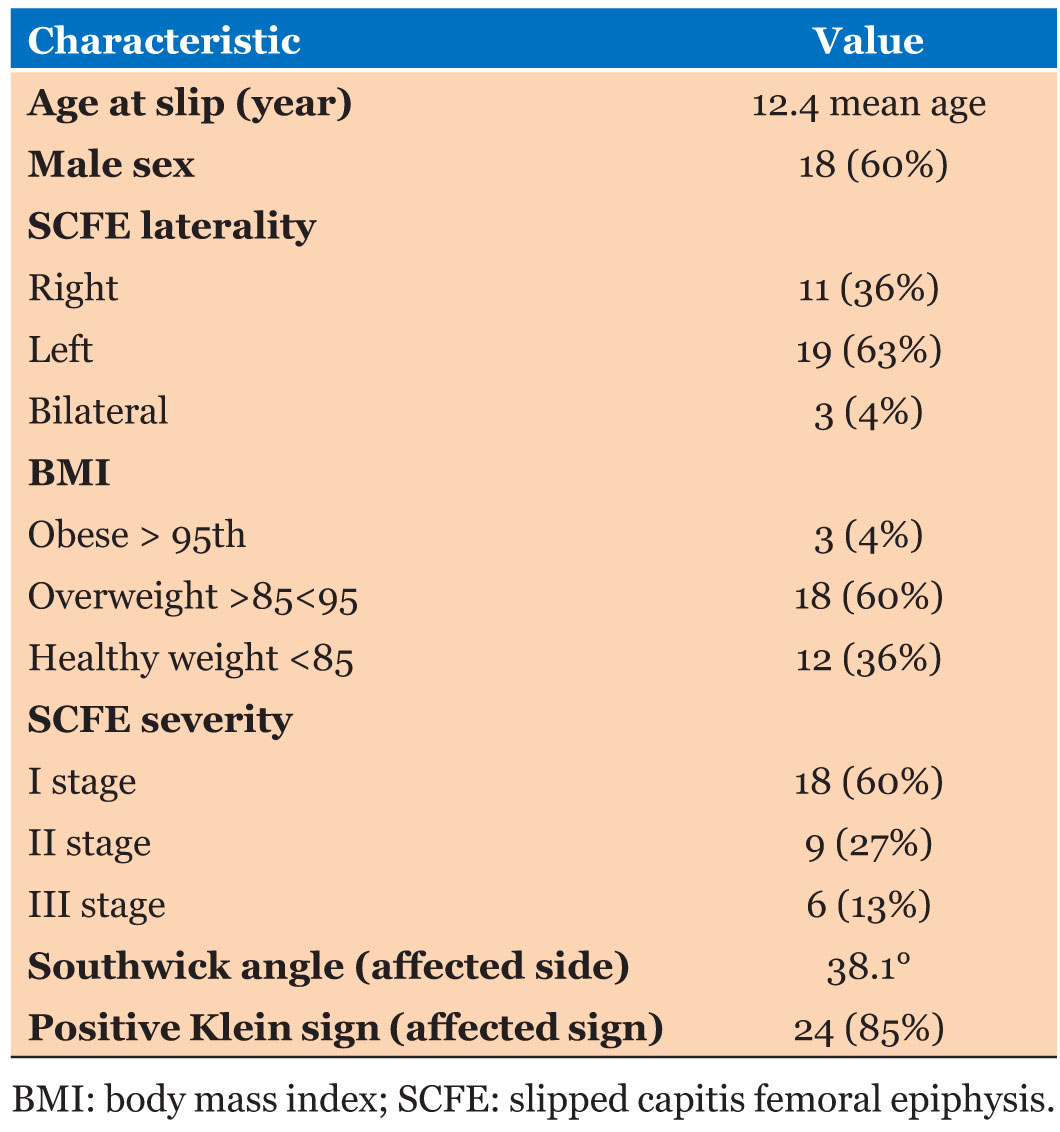
Our study is a monocentric retrospective clinical and radiographic study with a medium follow-up long-term work performed at the Regional Hospital of Bellinzona and Valleys, Reference Center Pediatric for the Canton of Ticino. At our Institute, 33 patients were operated between 1998 and 2017 with the diagnosis of epiphysiolysis hip. Table 1 summarizes the demographic features of the population examined.
All patients were operated with percutaneous fixation technique with a single screw, associated or not with closed reduction of slipping. The screw was positioned perpendicular to the physiques and center of the femoral head.
The degree of sliding allowed to classify a mild, moderate, and severe stage based on the value of the Southwick angle (considered pathological for values above 7°), measured on the “frog-leg lateral view” profile of both hips.
Epiphysiolysis was then defined according to the “unstable” Loden criteria if the path was not possible due to severe pain even with crutches.
Finally, we divided the epiphysiolysis into acute, if the symptoms had persisted for less than 3 weeks, chronic if >3 weeks, and acute on chronic if symptoms >3 weeks with the presence of acute exacerbation of pain.
The radiographic projections performed both at the first visit and during the follow-up are the AP radiography of the pelvis and the “frog-leg lateral view” projection of the bilateral hips (supine position with in flexion of about 45° and abduction of about 45°, knees flexed at 90° with the soles of the feet together (supine positioning, hip flexion of approximately 45 and abduction of approximately 45, knees flexed to about 90 with both feet placed together).
We also considered the new radiological classification method of Daniel et al. which relates the epiphyseal tubercle and its respective portion of metaphyseal bone to the lateral radiography which confirms the correlation with the degree of sliding of the epiphysis measured with the Southwick angle.
A clinical examination was performed to evaluate joint mobility in flexion-extension, abduction-adduction, and external-internal rotation associated with a form according to the Oxford hip score.
The radiological examination also allowed to evaluate signs of osteoarthritis according to the Tönnis classification and signs of femoroacetabular impingement, such as convexity at the junction between femoral head and neck, head flatness, osteophytes, and herniation pit. The following angles were also measured VCA (vertical-center-anterior), VCE (vertical-center-edge), AR (acetabular roof). Any surgical revision or removal of osteosynthesis media was noted.
Statistical analysis
A single observer analyzed and measured all pre-operative and follow-up radiographs in order to have a single measurement method.
Patients were analyzed based on number and percentage regarding population demographics, mean and standard deviation. Radiographic analysis the hip involved made use of the measurement of the Southwick angle. A descriptive analysis was made, with comparative analysis of each parameter on non-parametric Wilcoxon test for small samples. The significance threshold was seat p <0.05.
RESULTS
Thirty-three patients included in the study with an average follow-up of 7.7 years (minimum 3 years and maximum 11.5 years). The average age found is 12.4 years with a range between 8 and 15.8 years. The male sex is mainly involved with 60% of the cases, as well as the predominant side is the left (63%).
The estimated body mass index (BMI) identified 60% of overweight patients with a percentile between 85th and 95th and 4% of obese patients with percentile above 95th.
The average preoperative Southwick angle is 38.1° with a range between 25° and 65°. The degree of sliding severity was 60% at stage I (n = 18), 27% at stage II (n = 9), and 13% in stage III (n = 6). At the last clinical follow-up, we had complete hip mobility operated with a flexion-extension, abduction-adduction, and external-internal rotation without limitations.
The average global Oxford score is 47.2 points corresponding to good joint functionality unimpeded during daily life. At the last radiological follow-up the average AR angle was 13° (range 5–40°), VCE was 30° (13–55°), VCA was 30° (10–65°).
In addition, 10 patients had a grade 0 or 1 of osteoarthritis according to Tönnis. No patient presented clinical and radiological signs for femoroacetabular impingement.
DISCUSSION
The present study showed excellent efficacy in the treatment of femoral head epiphysiolysis with percutaneous fixation with a single screw, both for the little invasiveness of the surgical technique and for the results obtained.
The 33 patients included had a pre-operative Southwick angle of 38.1° and, following treatment, an Oxford hip score of 47.2 points was calculated. Even in the literature, as found by Hansson et al. [9] and by Monin et al. [10] in a study with 10 years of follow-up, a threshold value of 35–40° is set below which percutaneous fixation in situ is always recommended.
For more severe epiphysiolysis, with sliding angles >40°, the functional prognosis is worse, with associated increased risk of incurring osteoarthritis and femoroacetabular impingement.
In our series we did not observe any clinical and radiological signs for femoroacetabular impingement and in 30.3% of patients a grade 0-1 arthrosis according to Tönnis was found. These data are less in line with the literature.
Several studies evaluating ISF with long-term follow-up demonstrate an important rate of osteoarthritis despite early and optimal surgery.
Nectoux et al. [5], in a study with 222 cases of patients, operated on with a mean preoperative Southwick angle of 38.8°, they found a low rate of impingement (0.07%) but 88% of osteoarthritis grade 0-1 according to the classification of Tönnis; Wensaas et al. [6] report an osteoarthritis evolution in 28% of cases with an average follow-up of 33 years. Finally Murgier et al. [7] reported arthritic evolution in 22% of cases, grade II–III according to Tönnis, with a follow-up of 26 years.
Regarding the development of femoroacetabular impingement, Wensaas et al. [6] found a higher incidence of radiological signs of impingement after an isolated ISF and 37 years of follow-up compared to a control population without hip disease.
A possible hypothesis to explain this diversity in radiological evolution is based on the different and individual bone remodeling at the head-neck junction that occurs in each patient.
There are limits to our study. Firstly, as mentioned by authors, study involves small number of patients, due to the difficulty of contacting them posteriorly several years after surgery; secondly, the functional outcome examination using the Oxford hip score-12 is influenced by the subjectivity of the patients and does not include an objective physical examination; finally, our study does not have a control group that allows a comparison in functional and radiological terms.
CONCLUSION
The percutaneous screw fixation of slipped capital femoral epiphysis is a safe technique that does not need to open the joint and allows an anatomical reduction and good stability of the femoral epiphysis without any disadvantages. Although patients are satisfied at most recent follow-up, further long-term follow-up will be beneficial to assess the risk of developing impingement and secondary arthritic changes.
REFERENCES
1.
Herngren B, Stenmarker M, Vavruch L, Hagglund G. Slipped capital femoral epiphysis: A population-based study. BMC Musculoskelet Disord 2017;18(1):304. [CrossRef]
[Pubmed]

2.
Peck DM, Voss LM, Voss TT. Slipped capital femoral epiphysis: Diagnosis and management. Am Fam Physician 2017;95(12):779–84.
[Pubmed]

3.
Lehmann TG, Engesæter IØ, Laborie LB, Rosendahl K, Lie SA, Engesæter LB. In situ fixation of slipped capital femoral epiphysis with Steinmann pins. Acta Orthop 2011;82(3):333–8. [CrossRef]
[Pubmed]

4.
Mahran MA, Baraka MM, Hefny HM. Slipped capital femoral epiphysis: A review of management in the hip impingement era. SICOT J 2017;3:35. [CrossRef]
[Pubmed]

5.
Nectoux E, Décaudain J, Accadbled F, et al. Evolution of slipped capital femoral epiphysis after in situ screw fixation at a mean 11 years’ follow-up: A 222 case series. Orthop Traumatol Surg Res 2015;101(1):51–4. [CrossRef]
[Pubmed]

6.
Wensaas A, Svenningsen S, Terjesen T. Long-term outcome of slipped capital femoral epiphysis: A 38-year follow-up of 66 patients. J Child Orthop 2011;5(2):75–2. [CrossRef]
[Pubmed]

7.
Murgier J, de Gauzy JS, Jabbour FC, et al. Long-term evolution of slipped capital femoral epiphysis treated by in situ fixation: A 26 years follow-up of 11 hips. Orthop Rev (Pavia) 2014;6(2):5335. [CrossRef]
[Pubmed]

8.
Millis MB, Novais EN. In situ fixation for slipped capital femoral epiphysis: Perspectives in 2011. J Bone Joint Surg Am 2011;93 Suppl 2:46–51. [CrossRef]
[Pubmed]

9.
Hansson G, Billing L, Högstedt B, Jerre R, Wallin J. Long-term results after nailing in situ of slipped upper femoral epiphysis. A 30-year follow-up of 59 hips. J Bone Joint Surg Br 1998;80(1):70–7. [CrossRef]
[Pubmed]

10.
Monin JO, Gouin F, Guillard S, Rogez JM. Late results of the treatment of the slipped upper femoral epiphysis (26 cases with follow-up study over 10 years). [Article in French]. Rev Chir Orthop Reparatrice Appar Mot 1995;81(1):35–43.
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Marco Odorizzi - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Vincenzo De Rosa - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Alberto Mameli - Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Marco Odorizzi et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.